Is the Oxygen Index (OI) an Outdated Tool for ECMO Initiation?
Free ECMO & Critical Care Newsletter, please subscribe
I just returned from the SWAAC ELSO Conference in Abu Dhabi, where one roundtable discussion was titled: "Is OI an Outdated Tool?" This conversation challenged one of the longest-standing ECMO initiation markers—Oxygen Index (OI) > 40—and explored whether it still holds up in today’s practice.
As a respiratory therapist, I’ve always recognized that a good blood gas doesn’t always mean a good ventilator strategy. It wasn’t long ago that we routinely ventilated patients with 15 mL/kg tidal volumes and driving pressures that were way too high—and back then, we thought we were doing the right thing! The ABGs looked great, but we now know that we were causing massive ventilator-induced lung injury.
This same principle applies to OI as an ECMO threshold—it’s one piece of the puzzle, but ventilator settings play a huge role in making that number look better or worse than it really is.
What is the Oxygen Index (OI), and Why is it Used?
OI is a calculated measure of how much ventilatory support is required to maintain oxygenation. It is commonly used in pediatric and neonatal respiratory failure but applies to adults with severe ARDS.
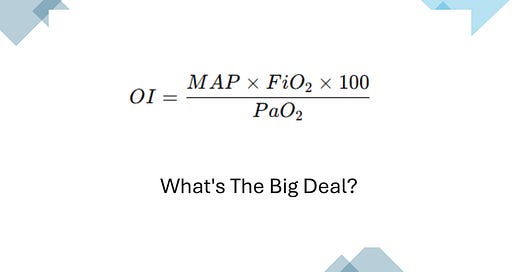
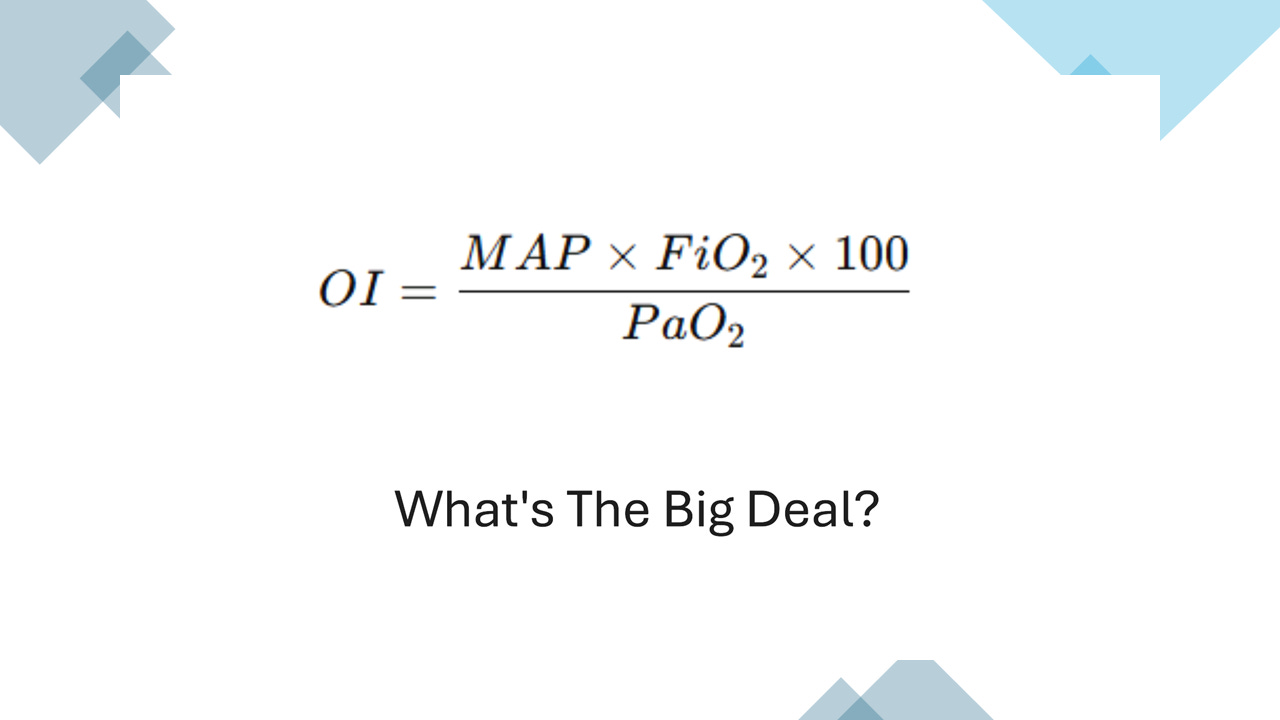
OI Formula:
OI=(MAP×FiO2×100)/PaO
Where:
MAP = Mean Airway Pressure (cmH₂O) from the ventilator
FiO₂ = Fraction of Inspired Oxygen (expressed as a decimal)
PaO₂ = Partial Pressure of Arterial Oxygen (mmHg)
Why Has OI Been Used for ECMO?
During the roundtable, it was mentioned that, historically, OI correlates with worsening oxygenation failure. It has been used to determine when conventional ventilation is failing and Nitric or ECMO should be considered.
OI < 5 Normal oxygenation
OI 10-20 Mild lung injury
OI 20-30 Moderate lung injury
OI > 30 Severe lung injury (possibly NO)
OI > 40 for several hours, then Historically,y a strong ECMO trigger
But does OI truly reflect the need for ECMO, or is it just another number that ventilator settings can manipulate?
The Roundtable Discussion: "Is OI an Outdated Tool?"
At the SWAAC ELSO Conference, experts debated whether OI should still be the primary trigger for ECMO initiation or if newer clinical decision-making strategies should take priority. Here are 4 takeaways I got, with some of my thoughts added:
1. A "Great" Blood Gas Doesn't Mean a Safe Ventilator Strategy
As I learned in the early days of being a Respiratory Therapist, a normal PaO₂ and CO₂ don’t mean the patient is okay. If those numbers were achieved with damaging ventilator settings (e.g., high tidal volumes, excessive PEEP, or high driving pressures), the lungs would still be in trouble.
Since MAP is part of the formula, aggressive ventilator settings (e.g., high PEEP, high inspiratory pressures) can artificially raise OI, making a patient appear sicker than they are.
Conversely, a lower OI doesn’t always mean stability—a patient may have rising CO₂, worsening lung compliance, or hemodynamic compromise.
2. ECMO Decisions Must Be Based on More Than OI Alone
Instead of using OI alone, many centers now incorporate a broader assessment, including:
PaO₂/FiO₂ Ratio (P/F Ratio) < 80. A strong indicator of severe hypoxemia
Ventilator Pressures & Compliance. A Driving Pressure > 15 cmH₂O, Pplat > 30 cmH₂O indicate worsening lung injury
Rising CO₂ and Respiratory Acidosis, a pH < 7.15 despite max vent settings, suggests hypercapnic failure.
Signs of Cardiovascular Compromise. A Rising lactate, hypotension, and shock indicate imminent organ failure
3. Timing is Everything—Waiting for OI > 40 Can Be Too Late
Some centers initiate ECMO at OI 30-35 if:
The trend is worsening despite optimal lung-protective settings.
There are signs of high ventilator-induced lung injury (VILI)
Hypercapnic respiratory failure is progressing.
4. What This Means for ECMO Practice
OI > 40 is still an important warning sign but should not be used in isolation. The best ECMO centers now:
Follow OI trends instead of a single-value
Consider ECMO at OI 30-35 if other failure signs are present.
Look at indicators like P/F ratio, ventilatory pressures, and organ function.
Final Thoughts
The roundtable discussion at SWAAC ELSO reinforced a key principle: ECMO decision-making must evolve beyond rigid OI thresholds. While OI remains valuable, today’s practice should focus on patient trends, overall lung mechanics, and organ function rather than a single number.
Free ECMO & Critical Care Newsletter
This website, lifesupport.training, offers this free newsletter covering ECMO, critical care, and exam prep insights.
I’m also working on premium content, including ELSO exam prep, ACLS/PALS/BLS/ATLS study materials, and ECMO summary sheets.
Sign up now to stay updated and get early access when premium content launches.
Acknowledgments:
Here is a list of tools and resources that assisted in creating this article and others. I developed three custom GPTs for specialized research:
OpenEvidence (Daniel Nadler and Zachary Ziegler, OpenEvidence)
GPT-4o/o1, Claude 3.5 Sonnet/Opus, Perplexity, Gemini 1.5 Flash
Grammarly for editorial and proofreading assistance (can't live without it)
Leonardo AI, DALL-E3 AI Image Generator, Microsoft Designer, and Adobe Express for generating images and visual content
Join my ECMO learning journey. As a novice, I simplify concepts to enhance my understanding, one article at a time.